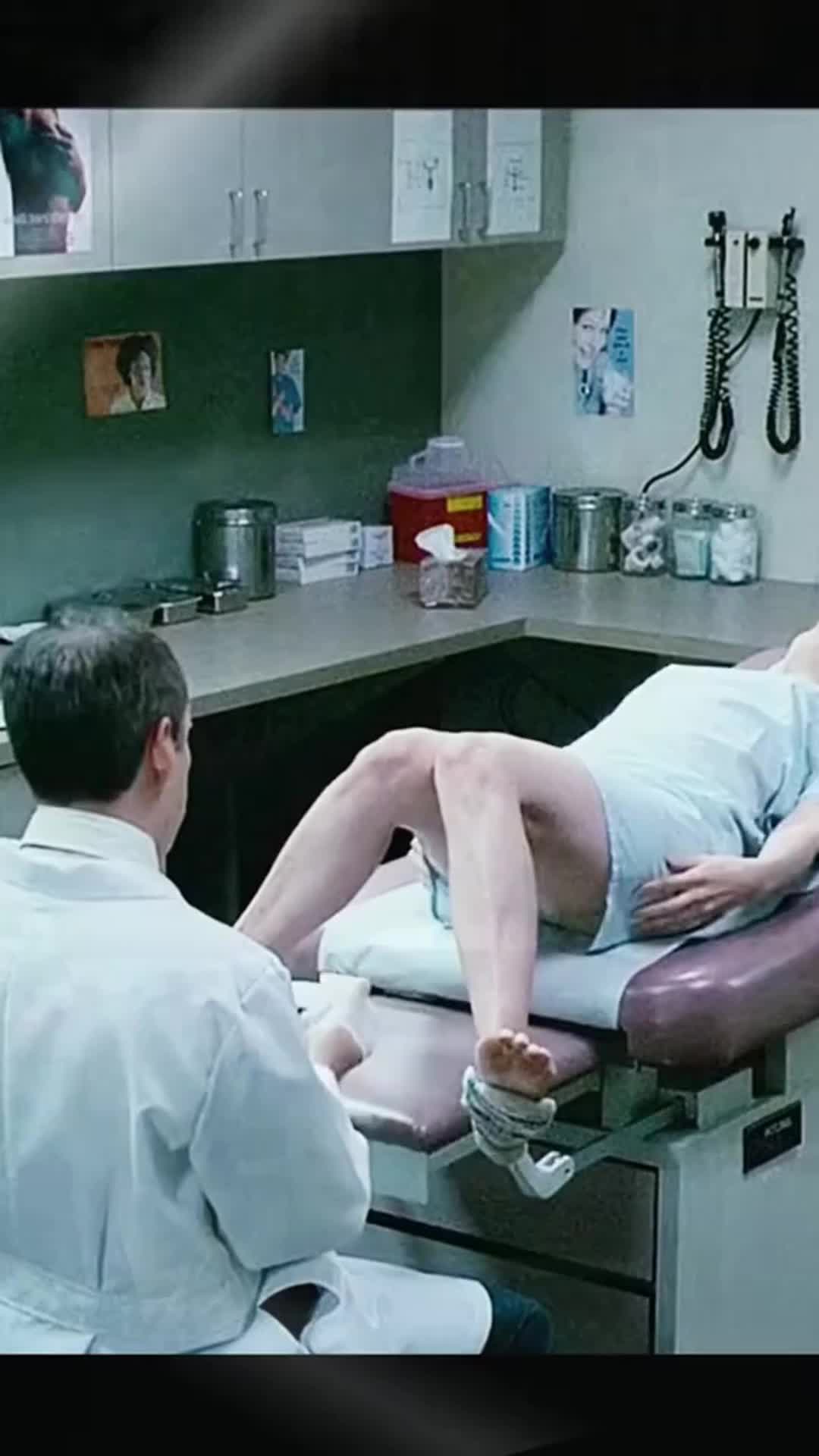
Carmen aiken of chicago made an appointment for an annual Physical Exam in July 2023, planning to get checked out and have Blood Work Done.
The Appointment was at a family medicine prectice run by university of illinois health. Aiken Said The Docor Recommended they Undergo a Pap Smear and Testing for sexually transmitted infctions. Aiken, who works for a nonprofit and use the pronoun, was also encouneded to get the hpv vaccine.
They’d tested Positive for HPV in 2019 and eventually cleared the virus but hadn’t gotten the vaccine to prevent infection.
“Sounds like a good idea,” Aiken, 37, recalled telling the doctor.
They Also Needed Some Lab Work – Part of Routine Monitoring for One Prescription. AFTER BEING EXAMINED, AIKEN SAID, they were directly to a different part of the Office Building to Get Blood Draw and Receive the first doses of the Vaccine before leaving.
Then the Bill for what aiken thought would be a freely exam: $ 1,430.
The Medical Procedure
The Services at Aiken’s Appointment Included A Pelvic Exam, A Vaccination and Blood Work to Check, Among Other Things, Glucose Levels and Liver Function.
A yearly Physical typical includes a variety of services, many that insurers are Required to Cover Under the Federal Afordable Care Act, Such As Revisionwing the Patient’s Health History, Screening for High Cholesterol and Performing a Pap Smear to Check the CERVIX for Signs of Cancer.
Updating immunizations is also a common and typically covered Service that a part of checkups. The Vaccine for HPV – The Human Papillomavirus – Provides Protection Against an Infection that Can Cause Several Types of Cancer. Federal Health Officials Recommend Being immunized for hpv at 11 or 12, though the vaccine also can be administrative late in life.
The final bill
It was $ 1,430.13.
That Broke Down to $ 1,223.22 for Lab Services and Pathology, plus $ 206.91 for “Professional Services,” which Included a Charge for A 40-Minute “High MDM” Outpatient Visit-Indication A High Level of “Medical Decision-Making”-as well as charges for administration. and vaccines.
A HOSPITAL PRICE TAG FOR BLOOD WORK
The Billing issue for aiken is that not all servings that might be provided as part of a yearly Physical necessarily will be covered by insurers as preventive care.
Someone Who Needs Blood Work for A Specific Medical Concern – As aiken Did, for Medication Monitoring – Could Be Required to Pay Part of the Bill. That’s TRUE IF The Blood Work is Performed During A Checkup Alongside Preventive Services.
Some Health Insurers Pay for Standard Blood Work as Part of A Prevention Visit. But that not always the case.
Aiken had purchas a health Insurance plan on the federal marketplace and though the visits to be covered at no cost.
When the Bill Came for More than $ 1,400, Aiken Thought, “How Did This Happen?”
They Said They Called Their Insurer, BlueCross Blueshield of Illinois, and THEN, AFTER AN INITIAL INQUIRY Went Nowhere, Filed an Appeal for the $ 1,223.22 Amout Owed for Lab Services, Thinking: “Surely, This is a Misterstanding.”
But the insurer sded with ui health’s stision that the blood work was prevenctive. In a Letter denying aiken’s appeal, bluecross blueshield of illinois said “The Labs were billed correctly as diagnostic.”
The Insure Decide Aiken was on the Hook for 50% of the Cost of Outpatient Labs performed in a hospital setting.
Dave van de walle, a spokesperson for BlueCross Blueshield of Illinois, Woupledn’t Discuss Aiken’s Bill.
Francesca Sacco, A UI Health Spokesperson, Said Aiken Scheduled the Appointment for “Medication Monitoring and to Obtain a Vaccine.
“Medication Monitoring is not consider a wellness benef under the afffordable care act,” she said.
SACCO ALSO SAID AIKEN’S LABS WERE SENT FOR PROCESSING TO UNIVERSITY OF Illinois Hospital, more than a mile from the family medicine practice.
That left aiken owing more. Hospitals typically Charge Much More than Doctors’ Offices or Independent Commercial Labs for the Same Tests.
The distinction between a preventive visits and a diagnostic one is important for billing purposes: it dictates who’s on the hook for the bill. A Preventive Visit Generally Comes at No Cost to Patients. But a visits for an ongoing medical wills is usablely classified as diagnostic, leaving the patient subject to copays and deductibles – or events charged for two separate appointments.
Patients Might not Notice a Difference in the Exam Room. Much of that nuance is determining by the medical provider and capured on the bill.
There’s the Still Confusion About Such Billing Matters 15 Years AFTER the ACA Prevention Services Protections took Effect, Accorting to Sabrina Corlette, A Founder and Co-Director of Georgetown University’s on Health Insurance Reforms.
“This is an Outrageous bill for what should have ben routine care,” Corlette Said. “People JUST DON’T HAVE THIS KIND OF MONE LYING AROUND.”
The resolution
After the insurer Denied the Billing Appeal, Aiken “Fell Down a Hole Into Despair About it for a while. And then someone Wise was, Like, you can pay it, and then stop thinking about it. ‘” “
So that’s what aiken did: “I put it on my credit card.”
SACCO SAID UI HEALTH WORKS WITH Insurers to Resolve Cost-Sharing Dispsal, “Howver, It is the Insurance Company’s Sole Discretion Whether A Service is Fully Covered or Subject to Cost-Sharing. A specific Portion of the Services Provided to the Patient.
The experience had had a lasting impact on aiken, who said last year they walked out of an urgent-core vister a doctor recommended a pap smear-Fearing that to do result in another big bill.
The Takeaway
Delaying or avoiding a cana lead to work outComes, which is why lawmakers tried to enure geeryLly woul no Nothing for preventive services Like immunizations under the aCa.
Yearly checkups are a key element of preventive care.
For instance, Most adults who never got the hpv Vaccine don’t know they’re still eligible, so is it critical to say of their options, Said Dr. Verda Hicks, a Gynecologist oncologist in Kansas City, Missouri.
The Vaccine Offers Protection Against Nine Types of HPV and Against Hpv-Relay Cancers in Men, SO FEDERAL CENTERS FOR DISEASE CONTROL AND PREVENTION RECOMMANS BOYS GET The Shot, Too.
“Get Vaccinated,” Hicks Said, Pointing Out the Difference It Makes for HPV. “We just do not have the Same tools for Many Other Cancers.”
But some insurance companies won’t cover the cost of the Vaccine For Some Older Patients -and the sun services might be subject to different Cost-sharaing rules Depending on whether they are conducted for prevention versus diagnosis.
Also, Price Can Vary Depending on Where You Go For Care and Where The Tests are performed. If you need a Blood test, ask that your doctor send the requisition to a commercial, in-network lab. People might not realize that labs drawn at a clinic could be sent to a hospital for testing, opening say to higher costs.
There hay been a push in congress to eliminate this price variation through “site-neutral” Payment police under which, Regardless of Location, the price for Routine Care to be reimbured at the Same Amount.
“Site-Neutral Reforms Potentially Have Significantly Reduced Carmen’s Expensses,” Said Christine Monahan, An Assistant Research Professor at Georgetown’s Center on Health Insurance Reforms.
Potentially upending the Current System: A Case before the supreme couldite eliminate the requirement that insurers cover preventive servings like vaccines and annual screenings at no cost. If the Justices – WHO Heard Oral Arguments April 21 -Side with the plaintiffs, Corlette Said, “THEN, we all potentially loose access to free, high-value preventive care. And that to be a real shame.”
Samantha Liss and Lauren Sausser are Reporters for KFF Health News.